Four years ago, Dr. Leslie Dempsey would never have talked about ACEs — adverse childhood experiences — with her patients. Now ACEs is a common topic. “Just as I don’t feel awkward asking someone if they smoke or do intravenous drugs, I don’t really feel awkward talking about their childhood traumas in a way that it relates to their health. It’s just integrated into obtaining background and social history,” she says.

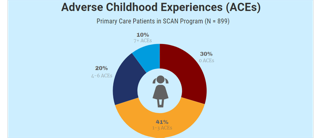
Dempsey is a physician in obstetrics who oversees a team at a bustling clinic staffed mostly by medical residents in Pueblo, CO. In October 2015, the clinic, known as the Southern Colorado Family Medicine clinic (SCFM) and housed at the St. Mary-Corwin Medical Center, began integrating ACEs science in a program called SCAN — Support, Connect and Nurture. Over 3.5 years, 899 patients, 23 medical residents, and two family development specialists participated in SCAN, a collaboration between the clinic, Catholic Charities and Chapin Hall at the University of Chicago. (Read about the SCAN program’s first year at the SCFM in this in-depth ACEs Connection article.)
Last week, a report was released about SCAN’s progress by Drs. Julie McRae and Tiffany Burkhardt, researchers at Chapin Hall at the University of Chicago. Among their findings, they learned that:
- ACEs predicted depression and poorer health in adulthood.
- Resiliency buffered the relationship between ACEs and depression — ACEs are a stronger predictor of depression among adults who reported low levels of resiliency. For example, patients with ACE scores of 4 or more ACEs had significantly lower resiliency scores than patients with an ACE score of up to 3.
- SCAN reduced stress in staff and helped providers get families the services they needed.
- Emergency department visit rates dropped from 1.08 to 0.84 visits per year on average, resulting in substantial cost savings.
ACEs comes from the groundbreaking Adverse Childhood Experience Study (ACE Study), first published in 1998 and comprising more than 70 research papers published over the following 15 years. The research is based on a survey of more than 17,000 adults and was led by Drs. Robert Anda and Vincent Felitti. The study linked 10 types of childhood adversity — such as living with a parent who is mentally ill, has abused alcohol or is emotionally abusive — to the adult onset of chronic disease, mental illness, violence and being a victim of violence. Many other types of ACEs — including racism, bullying, a father being abused, and community violence — have been added to subsequent ACE surveys. (ACEs Science 101; Got Your ACE/Resilience Score?)
The ACE surveys — the epidemiology of childhood adversity — is one of five parts of ACEs science, which also includes how toxic stress from ACEs affects children’s brains, the short- and long-term health effects of toxic stress, the epigenetics of toxic stress (how it’s passed on from generation to generation), and research on resilience, which includes how individuals, organizations, systems and communities can integrate ACEs science to solve our most intractable problems.
To measure resilience in their patients, the clinic used the Connor Davidson resiliency scale.
According to the report, patients were receptive to learning about their ACEs and resilience: “Most SCAN patients (91%) said they would recommend that others like them receive the SCAN service, particularly the portion of the visit that involved the ACE questionnaire. Participants discussed the benefits of the program in terms of the resources offered, support, and opportunity to reflect.” (See the attached report below.)
That result comports with Dempsey’s experiences. “Very few people we talked to about [ACEs] declined to take our questionnaire,” she says.
Key to the success of SCAN are the family development specialists. They meet the patient in the exam room, ask them if they’re willing to fill out ACEs and resiliency screeners and educate new parents and pregnant women in the clinic’s high-risk obstetrics clinic about their own ACEs and resiliency, according to a newly-released report by University of Chicago researchers.
The family development specialists also offer patients a variety of supports, including an onsite HealthySteps program, and offsite parenting education classes, housing and nutrition programs, many through the clinic’s partnering organization, Catholic Charities.
Chantalle Trujillo-Navarrete was one of the family development specialists involved at the beginning of the program. Before joining SCFM, she did similar work for Catholic Charities in Pueblo. She helped families navigate the shoals of unstable housing, hunger, job loss, and other crises until they reached an anchoring point. The SCAN project added the focus of preventing childhood trauma.
Trujillo-Navarette, who now works full time as a clinician and case manager in the clinic’s HealthySteps program, but still fills in for the other family development specialists when they’re unavailable, has seen big changes in how patients relate to her and the other family development specialists.

“When I first started here, our phones would never ring. We’d give our number out and there would be zero calls. And now we get phone calls from families ‘my car broke down’ or ‘I don’t have transportation, and I need to get the kids to school,” says Trujillo-Navarette, as examples of some of the five to 10 weekly calls they receive from patients.
She attributes the training in ACEs science that she and others received to the uptick in calls from patients, a testament to their patients’ increased trust in the family development specialists. “We’re not going in talking about them needing the services. We’re offering the service. We’re here to support them, not to tell them what to do, not to make them feel like they’re not parenting correctly or doing something right,” she says. “We really focus on meeting the family where they’re at.”
Trujillo-Navarette also says that part of her work has been educating patients about where to seek help when their children are ill. “We know that utilization of the emergency room in our community is pretty generational. A lot of families think ‘I took her to the ER the last time she fell down. I’m getting medical treatment so I’m doing the right thing,” she says. So now, she explains, they call when a child’s ill to ask if they should make a doctor’s appointment, go to urgent care, or to the ER.
That guidance has paid off, resulting in a small drop rates of emergency room visits with a resulting annual savings of $213,017, according to the report.
The work of the family development specialists has also resulted in less overall stress among the medical residents working in the clinic, a common problem among physicians, which left unabated can lead to physician burnout, according to the report and a growing body of research.

“The physicians talked about the extra support that having the resource of the family development specialist in the clinic provided to them, just being able to walk down the hall and ask questions right then and there and being able to connect a family to a service,” says McRae.
Dempsey agrees that family development specialists have eased up work flow not just for her, but for the entire clinic — ticking off examples of physician requests they respond to:
“Anywhere from, ‘We have a kid who just pooped into his diapers and mom doesn’t have any diapers with her’, to ‘Gramma just got awarded custody of three kids yesterday. And she has nothing. So now she’s in the clinic and she’s overwhelmed, and she has a newborn baby and two older siblings, and no car seat, and no baby supplies.’”
The family development specialists also make it easier for clinicians to be advocates for their patients when necessary, says Dempsey.
“We really feel like when we have to talk to social workers later about these high-risk moms, that we’re able to go to bat for them. Because we know they’re getting parenting classes. We know that they enrolled in counseling. We know that they’re in substance abuse treatment now. We’re really able to provide hard evidence of what our patients are doing to improve their lives and their parenting skills,” she says.




Comments (0)